In vitro TDAR
The aim of this Challenge is to develop a human in vitro T-cell dependent antibody response (TDAR) assay to assess the immune enhancement properties of immunomodulatory therapeutics during development.
Challenges briefing webinar
View the Challenges briefing webinar recording to find out more about this Challenge.
Phase 2 awarded
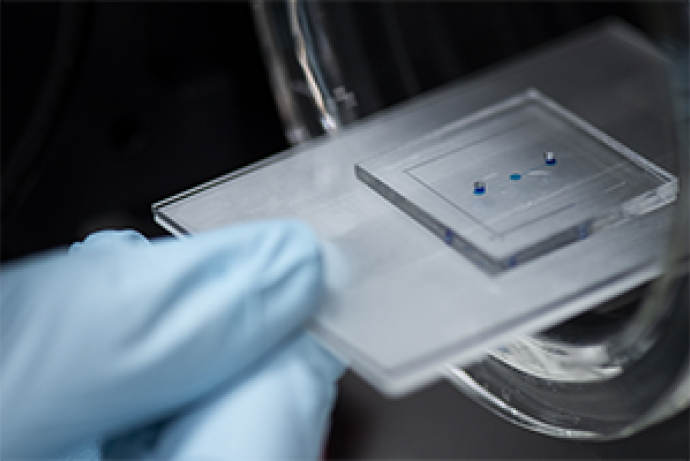
Phase 2 funding has been awarded to a multi-disciplinary team led by Dr Karla Queiroz, Mimetas B.V. to deliver the project TDAR-on-a-chip: a human in vitro HTS TDAR assay platform.
Phase 1 awarded
Three Phase 1 Awards were made to project teams led by:
- Dr Karla Queiroz, Mimetas BV, £100,000.
- Jun-Prof Dr Peter Loskill, Eberhard Karls University Tübingen, £100,000.
- Dr Qibo Zhang, University of Liverpool, £94,149.
Challenge launched
Sponsored by Bayer AG, GSK, Merck Healthcare KGaA and Novartis Pharma AG this Challenge aims to develop a human in vitro T-cell dependent antibody response (TDAR) assay to assess the immune enhancement properties of immunomodulatory therapeutics during development.
Background
Immune modulators
Immune modulators – defined as therapeutics that modify the immune response – are one of the fastest growing drug classes in preclinical drug development. They are being developed across multiple indications including viral diseases, autoimmunity and cancer immunotherapy. The cancer immunotherapy market is expected to grow to $106.6 billion in 2022 and reach $193bn in 2027 (Vision Gain report, 2018). Currently, there are around 2,720 immune modulating biologics and 1,179 immune modulating small molecules in development across all indications, and they are increasingly being used as combination therapies – for example, with immune checkpoint inhibitors in oncology indications (Cortellis databank analysis, Feb 2020).
Regulatory guidelines require that any potential adverse effects of new pharmaceutical agents on the immune system are evaluated prior to use. Immunotoxicological effects can occur either independent of the target of the drug (off-target) or, in the case of immune modulators, as exaggerated pharmacology (on-target). The impact of exaggerated pharmacology needs to be investigated in preclinical programmes, as excessive immune stimulation can lead to hypersensitivity reactions, increased propensity to develop autoimmunity or cytokine release syndrome (Brennan et al., 2018).
The TDAR assay
One of the gold standards recommended by regulatory guidelines to assess the immunotoxic effects of pharmaceuticals on immune function is the in vivo TDAR assay (European Medicines Agency, 2006 and 2011; Food and Drugs Administration, 1997 and 2020). It is a holistic assay that assesses the function and interplay of several cellular and humoral components of the immune system involved in mounting immune responses. The model antigen used to evoke an immune response in the assay, such as Keyhole Limpet Hemocyanin or Tetanus Toxin, is taken up by antigen presenting cells (APCs) such as dendritic cells, processed and presented in the context of major histocompatibility complex (MHC) molecules. Subsequently, T-cells recognise this specific MHC:peptide complex, become activated and in turn activate B-cells via both secreted cytokines and receptor interactions. Activated B-cells then differentiate into plasma cells that produce the appropriate antigen-specific antibodies. Any alteration to the antigen-specific responses detected in the in vivo TDAR assay can indicate potential effects of the therapeutic candidate on any of the involved cell types, including APCs, T-cells and B-cells.
Assessing immune enhancement
The TDAR assay is well-established for detecting immunosuppression due to off-target toxicity and on-target pharmacology in rodents and non-human primates (NHPs) for small molecules and biologics respectively. New immunomodulatory therapeutics can cause toxicity through on-target enhancement of the immune response (exaggerated pharmacology). For the assessment of immune enhancement, adaptations to the method, such as optimising the antigen concentration to induce a sub-maximal immune response, are required.
For biologics
The testing of biologics can usually only be conducted in NHPs due to the lack of target cross-reactivity in other species. When assessing immune suppression, the initiation of a robust immune response is required, however, to detect immune enhancement, a sub-maximal response is needed to look for increases to the immune response. NHPs show a high individual variability in their immune response and as a result, it is difficult to define a standardised antigen concentration to be used in the immunisation protocol of the TDAR assay for immune enhancement. If the evoked immune response is either too high or too low, the assay is insensitive in detecting an immune enhancing effect. Data obtained in such cases is difficult to interpret and could lead to an underestimation of the potential risk. Due to this variability, large numbers of NHPs are often required to assess immune enhancement in TDAR assays to ensure reliable results.
For small molecules
For small molecules, the TDAR assay is usually performed in rodents, typically rats. Immune modulating small molecule therapeutics are currently in early development but there is no established method to measure immune enhancement using the TDAR assay in rodents. As immune modulating small molecules progress in development, this will lead to an increased use of rodents to evaluate the immune enhancement properties of these therapeutics.
In vitro models
In vitro systems to detect immunosuppression have been reported but are not applicable for the assessment of immune enhancement (Fischer et al., 2011; Collinge et al., 2020), which is dependent on the proper matrices and spatial organisations of relevant immunological compartments. The system described by Fischer et al. (2011) uses rodent cells and may not translate to humans. A human lymphocyte activation assay that is similar to the in vivo TDAR assay has been reported (Collinge et al., 2020). However, the assay has only been evaluated using immunosuppressive compounds and uses cells from influenza-immunised donors, which means that only the secondary immune response can be measured.
With growing evidence that 3D in vitro immune microphysiological systems (MPS) such as the lymph node can be assembled (Shanti et al., 2018 and 2020; Sun et al., 2019), in principle there is a sound basis to adapt and validate these systems for the assessment of immune enhancement of immunomodulatory therapeutics. Immune responses initiated at different locations throughout the body are coordinated by secondary lymphoid organs, mainly the lymph nodes. The lymph nodes provide an optimal environment for the lymphocytes to effectively perform their function. A number of lymph-node-on-a-chip models have been reported, mostly in relation to chemotaxis, and the cellular response to chemokines (Shanti et al., 2018 and 2020). The use of such MPS models in pharmaceutical testing has however not been reported, especially in relation to T-cell responses.
The aim of this Challenge is to develop an in vitro human immune response assay to investigate the T-cell dependent antibody response for the preclinical assessment of immune enhancement of immunomodulatory therapeutics. As no species mimics the human immune response in all aspects a human in vitro immune response assay could better predict clinical outcomes (Bjornson-Hooper et al., 2019). Additionally, a system allowing for multiple replicate testing and benchmarking to already marketed therapeutics with known clinical effects would be advantageous, especially for poly-specific modalities (bi- or tri-specific antibodies) where identifying a relevant species for immunotoxicity and efficacy testing is problematic as these modalities may not cross react with any preclinical species.
3Rs benefits
A predictive human in vitro model developed through this Challenge could reduce the number of NHPs used to assess the immune enhancement properties of preclinical immunomodulatory biologics. Testing biologics usually requires 20 to 40 NHPs per study (typically cynomolgus macaques). Due to the high inter-animal variability in NHPs in their immune response in the in vivo TDAR assay studies, large animal numbers (n=10 per group) compared to standard toxicology studies (n=4 to 6 per group) are required to draw robust conclusions (Lebrec et al., 2011 and 2014). Study designs are not standard and are defined by the mechanism-of-action and pharmacokinetics of the therapeutic under investigation. For example, a study may include up to three dose groups plus a vehicle control, with up to ten animals per group. The immunisation schemes, sampling and analytical methods used are specific to the therapeutic under investigation. Commonly used antigens include Keyhole Limpet Hemocyanin, Tetanus Toxin or Hepatitis B antigen and read-outs of the immune response include measuring antigen-specific IgM and IgG antibody titres, numbers of antigen-specific B and T-cells.
There is currently no established method to assess immune enhancement in the rodent TDAR assay. As immune modulating small molecules progress in development, a human in vitro model could prevent the development of rodent models for assessing immune enhancement.
Once a robust and reliable model has been developed to detect immune enhancement it also has the potential to be adapted to detect immunosuppressive effects of pharmaceuticals and environmental chemicals (Boverhof et al., 2014), and could further replace the regulatory requirement for the use of rodents and reduce the number of NHPs used for immune function safety testing.
Full Challenge information
Assessment information
Review Panel membership
| Name | Institution |
| Professor Ian Kimber (Chair) | University of Manchester |
| Dr Pascale Buchmann (Sponsor) | Bayer AG |
| Dr Pelin Candarlioglu (Sponsor) | GSK |
| Dr Philip Hewitt (Sponsor) | Merck Healthcare KGaA |
| Dr Hannah Morgan (Sponsor) | Novartis Pharma AG |
| Professor Mark Coles | University of Oxford |
| Professor Matthias Eberl | Cardiff University |
| Professor Amir Ghaemmaghami | University of Nottingham |
| Professor John Greenman | University of Hull |
| Dr Michelle Linterman | Babraham Institute |
| Mr Colin Roberts | BioCity |
| Professor Pavel Tolar | The Francis Crick Institute |
| Professor Christoph Wuelfing | University of Bristol |