Cytokines
The aims of this Challenge were to develop in vitro human cell-based models for the testing of antibody-based therapeutics that would allow the prediction of human cytokine release and furthermore, to develop a parallel assay with cells from non-human primate (e.g. cynomolgus monkey) that could predict cytokine release in preclinical safety assessment.
Professor Martin Glennie and his team at the University of Southampton have successfully developed a simple and reproducible human immune cell based laboratory assay which allows the prediction of whether or not a monoclonal antibody (mAb) will cause harmful side effects in human subjects.
Publication
Hussain K et al. (2022). HIF activation enhances FcγRIIb expression on mononuclear phagocytes impeding tumor targeting antibody immunotherapy. Journal of Experimental & Clinical Cancer Research 41: e131. doi: 10.1186/s13046-022-02294-5
Publication
Hargreaves CE et al. (2015). Evaluation of High-Throughput Genomic Assays for the Fc Gamma Receptor Locus. PLoS One 10(11): e0142379. doi:10.1371/journal.pone.0142379.
Challenge completed
Professor Martin Glennie and the team from Southampton have successfully developed a simple and reproducible human immune cell based laboratory assay which allows the prediction of whether or not a monoclonal antibody (mAb) will cause harmful side effects in human subjects. The assay correctly predicts that mAbs which target human T cells have the potential to cause more harmful side effects in comparison to mAb which target the cancer cells directly. This novel testing method has the potential to increase the accuracy of predicting mAb induced harmful side effects and could be used alongside the suites of tests used to assess the safety of new therapeutic mAbs in humans.
Publication
Hussain K, Hargreaves CE, Roghanian A, et al. (2015). Upregulation of FcγRIIb on monocytes is necessary to promote the superagonist activity of TGN1412. Blood 125(1): 102-10. doi:10.1182/blood-2014-08-593061.
Challenge awarded
A team led by Professor Martin Glennie from the University of Southampton has been awarded £500k to deliver the project: Improving the predictive capacity of in vitro cytokine release assays to reduce animal use and drug attrition.
Challenge launched
Sponsored by Huntingdon Life Sciences (now Envigo), the Cytokines Challenge aims to develop in vitro human cell-based models for the testing of antibody-based therapeutics that will allow the prediction of human cytokine release, and reduce animal use and drug attrition.
Background
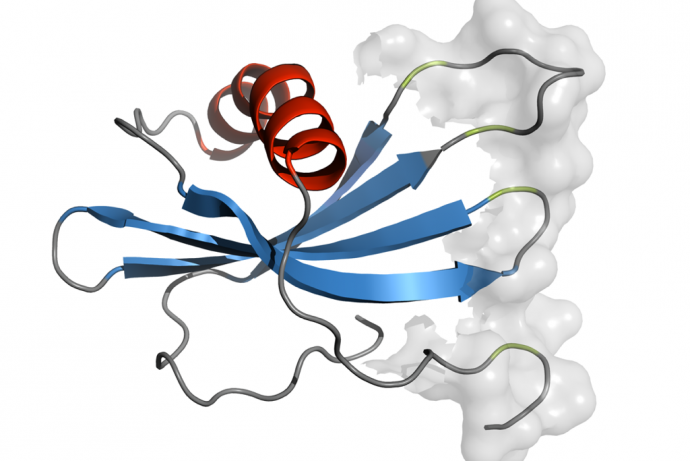
Cytokines are soluble signalling molecules which are released by cells of the immune system in response to antigen binding. Large molecule therapeutics such as antibodies can also trigger cytokine release and immune cell activation either directly by their V regions or by Fc regions binding to Fc receptors. A severe example of this was seen in the trial of TGN1412, an anti-CD28 IgG4, which activated T-cells resulting in massive cytokine generation and severe pathology in the volunteers that received it.
The in vivo testing of biologics, such as monoclonal antibodies, is a regulatory requirement with the cynomolgus monkey being the most commonly used species. Whilst this monkey is used in toxicity studies for a range of drugs, it has poor predictivity for the potential of antibody-induced cytokine release in humans. This may be in part due to differences in the expression of antigens such as CD28, the lower affinity of the cynomolgus FcR for human Fc or the presence of regulatory signalling molecules that humans lack such as CD33-related Siglec.
The lack of a standard format for these assays in combination with the poor predictive value of the current models has highlighted the need for a new generation model that will be sensitive and predictive of clinical outcome, and will therefore inform both candidate selection and be predictive of toxicology in preclinical or clinical studies.
3Rs benefits
Biologics form approximately 30% of the global drugs pipeline. Immune responses caused by these drugs, including desired pharmacology and adverse events are assessed in preclinical studies, primarily using the cynomolgus monkey. Depending on the drug, the therapeutic area and company practices up to 144 monkeys may be used in a standard toxicology package for biologics. Immune responses are assessed either as part of the standard toxicology package or as standalone studies. In vitro assays which accurately predict immune responses, including the likelihood of a cytokine storm, would reduce the number of monkeys used by avoiding drugs which are destined to fail on safety or efficacy grounds being taken into preclinical studies.
Additional 3Rs benefits include:
- Screening and optimising molecules prior to preclinical studies to avoid unnecessary use of animals. For instance, a robust in vitro screen for a monoclonal antibody could show whether engineering was needed to increase potency (if cytokine release is not stimulated enough) or reduce toxicity (if cytokine release is too high or not part of the expected pharmacology) prior to animal studies.
- Integration into the testing paradigm for biosimilars or manufacturing changes to use fewer (if any) animals for approval.
- Providing information on the mechanism of action and/or potency which could be used to inform study designs allowing fewer animals to be used and avoiding doses which result in significant adverse events or mortality.
Challenge winner
Project team led by:
Full Challenge Information
The aim of this Challenge was to develop robust assays that predict human toxicity for monoclonal antibody (mAb) therapy and thereby reduce the need for pre-clinical animal testing. Current pre-clinical animal models are aslo poorly predictive for Cytokine Release Syndrome (CRS) in humans, as exemplified by the ‘TeGenero’ incident where primate studies gave no indication of human adverse events.
In vitro assays which reliably predict human toxicity would dramatically reduce testing in animals- potentially to just to those required for minimal toxicity testing. These in vitro tests might also be particularly useful for the development of bio-similars where it is likely that efficacy and toxicity will be the same as the original therapy, but due to the underlining concerns that biosimilars are made in different clones and thus may behave differently, similar performance of the original therapy and the biosimilar in in vitro testing would be strong evidence that further animal tests would not be needed. In vitro testing would also provide insight into the mechanisms of action of a mAb and the option to further engineer to refine function via modification of the antibody.
Several leukocyte based assays were developed, and following discussion with the Sponsor, the team at University of Southampton validated one of these assays with the intention to use it to evaluate toxicity for a wide range of mAbs. The Cytokine Release Assay (CRA) assay was highly reproducible and correctly predicted that T cell targeting mAbs like TGN1412 have the potential to cause more severe toxicity and in comparison to non-T cell targeting mAbs like Avastin.
Furthermore, cynomolgus macaque peripheral blood mononuclear cells (PBMCs) reacted in a similar manner to human PBMCs in response to TGN142 stimulation in the CRA, providing the potential to reduce the need for cynomolgus macaques PBMCs to predict mAb induced toxicity in humans.
Further collaborative work will continue between, HLS and the University of Southampton if HLS chooses to commercialise the CRA developed by this project. There is a possibility that the testing of the potential of novel mAbs (in development), to cause CRS using the CRA developed by this project may be offered as a service to potential clients in the future by either HLS or the University of Southampton.