The cancer research field aims to improve treatment efficacy by understanding the molecular and cellular complexities of cancers, especially those with poor outcome. However, the field is hampered by the lack of reliable and standardised human cancer models that represent the human disease. Researchers at QMUL have developed, characterised and validated ex vivo human cancer models, as Experimental Cancer Medicine Platforms (ECMPs) for pancreatic cancer. The models provide an unprecedented opportunity to study, and develop therapies to treat, human malignancy in its native environment ex vivo, without using animals. Partners are sought to develop and expand the ECMPs across various cancer types, and validate the platform for preclinical drug development.
There are two key areas in tumour biology that must be considered when developing models to study the disease – tumour heterogeneity and the tumour microenvironment (TME).
Cancer heterogeneity is not only generated by genetically distinct subclones within each tumour, but also driven by phenotypic and functional heterogeneity within each of these subclones (Yachida et al., 2010; Garcia-Silva et al., 2013). These epigenetically defined phenotypes are responsible for intraclonal heterogeneity (Hermann et al., 2009; Hermann et al., 2008; Hermann et al., 2007; Li et al., 2007) including a functionally defined subset of so-called cancer stem cells (CSCs). The researchers at Barts Cancer Institute QMUL have provided conclusive evidence that these CSCs represent the root of the disease by giving rise to all differentiated progenies within each cancer subclone (Hermann et al., 2007; Cioff et al., 2015a; Lonardo et al., 2011; Miranda-Lorenzo et al., 2014; Sancho et al., 2015). Importantly, CSCs are essential for the metastatic behaviour of tumours and, due to their inherent chemoresistance, represent an important source for disease relapse (Hermann et al., 2007; Lonardo et al., 2011; Gallmeier et al., 2011; Hermann et al., 2010; Mueller et al., 2009; Merlos-Suarez et al., 2011).
The TME comprises many different cell types including cancer-associated fibroblasts (Bachem et al., 2005; Lonardo et al., 2012), endothelial cells and immune cells (Farrow et al., 2004; Chu et al., 2007) and a complex extracellular matrix (ECM). Apart from providing a mechanical barrier and structural support for tumour growth, dynamic interactions between malignant and stromal cells in the TME are critical for malignant cell growth, metastases and drug responses. To date, little is known about how the cells and matrix of the TME influence malignant cells (Rhim et al., 2014; Ozdemir et al., 2004; Kraman et al., 2010). Importantly, the researchers at QMUL have already shown that CSCs are influenced by their TME via multiple paracrine secreted factors affecting their aggressiveness, metastatic activity and drug resistance (Lonardo et al., 2011; Lonardo et al., 2012; Sainz et al., 2015; Cioffi et al., 2015b; Sainz et al., 2014).
Current cancer models, to examine drug responses, include cell lines, organoids or, more recently, in vivo patient-derived xenograft (PDX) models. Numerous new treatments have been developed based on these models and progressed into the clinic, where disappointingly the drugs failed or the results were highly variable among larger cohorts. The main reason for this high failure rate is because current models do not adequately reflect the cellular and temporal complexity of human cancer. Specifically, they insufficiently recapitulate the underlying hierarchical organisation, including CSCs and their progeny, do not include the multiple elements of the human tumour microenvironment, and rarely represent advanced metastatic cancer.
References
- Bachem MG, Schunemann M, Ramadani M, et al. (2005). Pancreatic carcinoma cells induce fibrosis by stimulating proliferation and matrix synthesis of stellate cells. Gastroenterology 128(4): 907-21. doi:10.1053/j.gastro.2004.12.036.
- Cioffi M, Trabulo SM, Sanchez-Ripoll Y, et al. (2015a). The miR-17-92 cluster counteracts quiescence and chemoresistance in a distinct subpopulation of pancreatic cancer stem cells. Gut 64(12): 1936-48. doi:10.1136/gutjnl-2014-308470.
- Cioffi M, Trabulo S, Hidalgo M, et al. (2015b). Inhibition of CD47 Effectively Targets Pancreatic Cancer Stem Cells via Dual Mechanisms. Clin Cancer Res 21(10): 2325-37. doi:10.1158/1078-0432.CCR-14-1399.
- Chu GC, Kimmelman AC, Hezel AF et al. (2007). Stromal biology of pancreatic cancer. J Cell Biochem 101(4): 887-907. doi:10.1002/jcb.21209.
- Farrow B, Sugiyama Y, Chen A, et al. (2004). Inflammatory mechanisms contributing to pancreatic cancer development. Ann Surg 239(6): 763-9. doi:10.1097/01.sla.0000128681.76786.07.
- Gallmeier E, Hermann PC, Mueller MT, et al. (2011). Inhibition of ataxia telangiectasia- and Rad3-related function abrogates the in vitro and in vivo tumorigenicity of human colon cancer cells through depletion of the CD133(+) tumor-initiating cell fraction. Stem Cells 29(3): 418-29. doi:10.1002/stem.595.
- Garcia-Silva S, Frias-Aldeguer J, Heeschen C. (2013) Stem cells & pancreatic cancer. Pancreatology 13(2): 110-3. doi:10.1016/j.pan.2012.12.003.
- Hermann PC, Bhaskar S, Cioffi M, et al. (2010). Cancer stem cells in solid tumors. Semin Cancer Biol 20(2): 77-84. doi:10.1016/j.copbio.2007.10.007.
- Hermann PC, Mueller MT, Heeschen C. (2009). Pancreatic cancer stem cells--insights and perspectives. Expert opinion on biological therapy 9(10): 1271-8. doi: 10.1517/14712590903246362.
- Hermann PC, Huber SL, Heeschen C. (2008) Metastatic cancer stem cells: a new target for anti-cancer therapy? Cell Cycle 7(2): 188-93. doi:10.4161/cc.7.2.5326.
- Hermann PC, Huber SL, Herrler T, et al. (2007). Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell 1(3): 313-23. doi: 10.1016/j.stem.2007.06.002.
- Kraman M, Bambrough PJ, Arnold JN, et al. (2010). Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-alpha. Science 330(6005): 827-30. doi:10.1126/science.1195300.
- Lonardo E, Hermann PC, Mueller MT, et al. (2011). Nodal/Activin signaling drives self-renewal and tumorigenicity of pancreatic cancer stem cells and provides a target for combined drug therapy. Cell Stem Cell 9(5): 433-46. doi:10.1016/j.stem.2011.10.001.
- Lonardo E, Frias-Aldeguer J, Hermann PC, et al. (2012). Pancreatic stellate cells form a niche for cancer stem cells and promote their self-renewal and invasiveness. Cell Cycle 11(7): 1282-90. doi:10.4161/cc.19679.
- Li C, Heidt DG, Dalerba P, et al. (2007). Identification of pancreatic cancer stem cells. Cancer Res 67(3): 1030-7. doi: 10.1158/0008-5472.CAN-06-2030
- Merlos-Suarez A, Barriga FM, Jung P, et al. (2011). The intestinal stem cell signature identifies colorectal cancer stem cells and predicts disease relapse. Cell Stem Cell 8(5): 511-24. doi:10.1016/j.stem.2011.02.020.
- Miranda-Lorenzo I, Dorado J, Lonardo E, et al. (2014). Intracellular autofluorescence: a biomarker for epithelial cancer stem cells. Nat Methods 11(11): 1161-9. doi:10.1038/nmeth.3112.
- Mueller MT, Hermann PC, Witthauer J, et al. (2009). Combined targeted treatment to eliminate tumorigenic cancer stem cells in human pancreatic cancer. Gastroenterology 137(3): 1102-13. doi:10.1053/j.gastro.2009.05.053.
- Ozdemir BC, Pentcheva-Hoang T, Carstens JL, et al. (2014). Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell 25(6): 719-34. doi:10.1016/j.ccr.2014.04.005.
- Rhim AD, Oberstein PE, Thomas DH, et al. (2014). Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell 25(6): 735-47. doi:10.1016/j.ccr.2014.04.021.
- Sainz B Jr., Alcala S, Garcia E, et al. (2015). Microenvironmental hCAP-18/LL-37 promotes pancreatic ductal adenocarcinoma by activating its cancer stem cell compartment. Gut 64(12): 1921-35. doi:10.1136/gutjnl-2014-308935.
- Sainz B Jr., Martin B, Tatari M, et al. (2014). ISG15 is a critical microenvironmental factor for pancreatic cancer stem cells. Cancer Res 74(24): 7309-20. doi:10.1158/0008-5472.CAN-14-1354.
- Sancho P, Burgos-Ramos E, Tavera A, et al. (2015). MYC/PGC-1alpha Balance Determines the Metabolic Phenotype and Plasticity of Pancreatic Cancer Stem Cells. Cell Metab 22(4): 590-605. doi:10.1016/j.cmet.2015.08.015.
- Yachida S, Jones S, Bozic I, et al. (2010). Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature 467(7319): 1114-7. doi:10.1038/nature09515.
Several technological advances from the researchers at QMUL overcome these limitations, enabling development of highly predictable ex vivo ECMPs incorporating human CSCs and human TME. These advances include:
- Developing technology to track and isolate CSCs, at highest purity, from various cancers including pancreatic, breast, colorectal and lung cancer by their inherent autofluorescence (Miranda-Lorenzo et al., 2014).
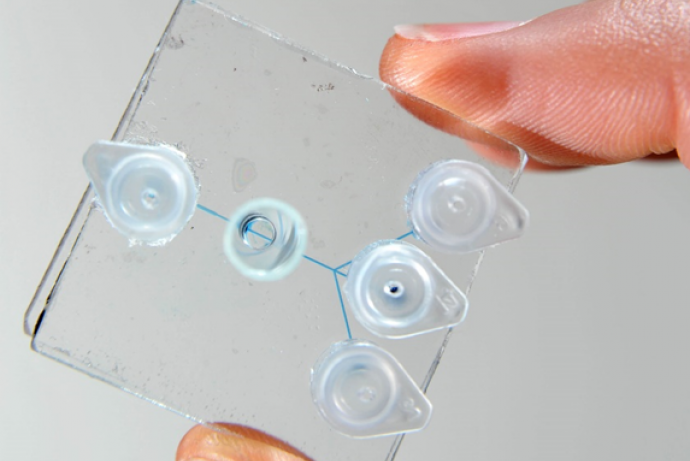
- Advancing a platform for the isolation of metastatic CSCs as the most aggressive subtype of CSCs from the circulating blood, thus providing repeatable access to viable biological material in unresectable patients (Clausell-Tormos et al., 2014).
- Establishing ultra-low-input protocols for transcriptomic, epigenomic and proteomic profiling of rare CSCs.
- Reconstructing faithfully the tumour microenvironment by introducing essential cellular components of the stroma into a synthetic niche (Lonardo et al., 2012; Cioffi et al., 2015b; Sainz et al., 2014; Sainz et al., 2015; Feig et al., 2015).
Based on the above state-of-the-art developments in the researchers lab, they have developed basic ECMPs that have already been validated for ex vivo drug response screening with particular emphasis on the elimination of the contained CSCs (ScanCSCTM). The platform utilises the inherent autofluorescence of CSCs, which can be constantly tracked in real time and is thus ideal for drug response screens (Miranda-Lorenzo et al. 2014). ScanCSCTM is a prototypic ECMP for pancreatic cancer, which utilises freshly isolated primary cancer cells derived directly from patients. The model not only provides drug response data for CSCs, but also for their differentiated progenies, non-CSCs. This platform has been developed for CSC-centred drug response profiling using compounds that are applicable to the clinic in order to select the most effective treatment for individual patients (precision medicine). The model can also assess compounds that hold potential as CSC-targeting agents, both as single agents and as multimodal treatment approaches. Currently, a 384-well format is used with 200 CSCs and 800 differentiated progenies per well embedded in ECM. This can be further miniaturised to a 1,536-well format requiring only 50 CSCs as the starting population and thus allow large-scale drug response screens for a representative panel of patient-derived tumours. Hits are identified based on efficacy (>50% reduction in autofluorescence [=CSC content]) combined with a >50% decline in cell viability over 72h of treatment as instructed by in vivo validation studies in pancreatic cancer.
References
- Clausell-Tormos J, Azevedo MM, Miranda-Lorenzo I, et al. (2014). Nano-Volume Well Array Chip for Large-Scale Propagation and High-Resolution Analysis of Individual Cancer Stem Cells. J Nanomed Nanotechnol 5(191): 1000191-98. doi:10.4172/2157-7439.1000191.
- Cioffi M, Trabulo S, Hidalgo M, et al. (2015b). Inhibition of CD47 Effectively Targets Pancreatic Cancer Stem Cells via Dual Mechanisms. Clin Cancer Res 21(10): 2325-37. doi:10.1158/1078-0432.CCR-14-1399.
- Feig C, Gopinathan A, Neesse A, et al. (2012). The pancreas cancer microenvironment. Clin Cancer Res 18(16): 4266-76. doi:10.1158/1078-0432.CCR-11-3114.
- Lonardo E, Frias-Aldeguer J, Hermann PC, et al. (2012). Pancreatic stellate cells form a niche for cancer stem cells and promote their self-renewal and invasiveness. Cell Cycle 11(7): 1282-90. doi:10.4161/cc.19679.
- Miranda-Lorenzo I, Dorado J, Lonardo E, et al. (2014). Intracellular autofluorescence: a biomarker for epithelial cancer stem cells. Nat Methods 11(11): 1161-9. doi:10.1038/nmeth.3112.
- Sainz B Jr., Alcala S, Garcia E, et al. (2015). Microenvironmental hCAP-18/LL-37 promotes pancreatic ductal adenocarcinoma by activating its cancer stem cell compartment. Gut 64(12): 1921-35. doi:10.1136/gutjnl-2014-308935.
- Sainz B Jr., Martin B, Tatari M, et al. (2014). ISG15 is a critical microenvironmental factor for pancreatic cancer stem cells. Cancer Res 74(24): 7309-20. doi:10.1158/0008-5472.CAN-14-1354.
The researchers at QMUL have created a unique and highly collaborative environment providing leading expertise in stem cell biology, TME and rare cell handling technologies. Partner(s) are sought to facilitate the further development of this platform and expand it across various cancer types, improve SOPs and validate the ECMPs for preclinical drug development and precision medicine. The partner(s) would ideally also have a larger panel of candidate drugs that could be tested and shortlisted using this platform.
The partner(s) will join an innovative and multidisciplinary team, providing an excellent opportunity to be part of the development and validation of a novel platform for experimental cancer medicine. The initial exploration focuses on drug response screening in order to prioritize compounds with the ability to eradicate CSCs as the most tumourigenic compartment in the tumour. Subsequently, the platforms can be used in the clinical setting for ex vivo drug response screens in order to select patients bearing the highest likelihood to respond to new treatment strategies and therefore should be primarily enrolled in respective clinical trials. Eventually, the platforms will also be of interest to health care providers in order to establish true precision medicine approaches.
Information about IP
There are currently no IP issues related to this platform. The researchers are open to discuss how future IP will be shared.
These ECMPs represent an innovative method for testing compounds without the use of animals in preclinical studies that can be easily expanded to compounds with different mechanism of action. Once validated, the system can be applied for: a) comprehensively studying CSC biology ex vivo; b) small- to large-scale drug screening efforts, and c) real-time evaluation of novel CSC-targeting therapeutics as a prelude to developing new treatment strategies and stratification for clinical trials. This system has two main features rarely considered in current 3D methods: intratumoural heterogeneity as well as inherent chemoresistance and tumourigenicity provided by the contained subpopulation of CSCs. These ECMPs will also provide important logistic advantages over current in vivo models including less biological variation due to more standardised conditions. In vivo models are too time-consuming and require considerable resources, and cannot be scaled up. As such, the use of the researchers ECMP will significantly reduce the number of mice used by at least 50%. Within the Barts Cancer Institute alone, half of the mouse work relates to early drug testing efforts. Thus, the researchers will potentially reduce the annual usage of experimental animals from 16,000 to 8,000. In addition, ECMP will also apply to collaborations with the pharmaceutical industry in testing and triaging novel anti-cancer agents, thus further reducing the use of animals outside of academia.