Inhalation Translation
This Challenge aimed to enable the longitudinal and non-invasive assessment of inflammation and foamy macrophages (FM) toxicity in the same animal through a series of dose-escalation stages. It required (i) the development of translational tools to assess FM modulation and inflammation in a longitudinal manner in rodent lungs (primarily the rat) and (ii) better insight into FM status and functionality as a response to drug inhalation.
To solve the Challenge, a team led by Dr Ben Forbes, Kings College London, developed an in vitro assay and refined in vivo model to reduce the use of animals to identify compounds with the potential to induce inflammation and foamy macrophage toxicity.
Publication
Forbes B (2018). Research activities following a Drugs in the Lungs Network workshop on induced alveolar macrophage responses. Inhalation Magazine.
Challenge completed
Through the Inhalation Translation Challenge, the team at Kings College London has developed an in vitro assay and refined in vivo model to reduce the use of animals to identify compounds with the potential to induce inflammation and foamy macrophage toxicity.
Conference presentation
Association of Inhalation Toxicologists Meeting 2017 (Copenhagen, Denmark)
- Oral presentation: Investigating the impact of macrophage polarization on alveolar macrophages in vitro.
- Oral presentation: Alveolar Macrophage Responses to Inhaled Medicines.
Conference presentation
Drug Delivery to the Lungs Conference 2017 (Edinburgh, UK)
A Study to Investigate the Ability of Inhaled Amiodarone to Induce ‘Foamy’ Alveolar Macrophages in Male Wistar Han Rats.
Publication
Hoffman E, Patel A, Ball D, et al. (2017). Morphometric Characterization of Rat and Human Alveolar Macrophage Cell Models and their Response to Amiodarone using High Content Image Analysis. Pharmaceutical research 34(12): 2466-2476. doi.org/10.1007/s11095-017-2176-5.
Conference presentation
American Society for Mass Spectrometry Annual Conference 2016 (Texas, USA)
Large scale, multi-instrument MALDI-MSI study into lipidosis in inhalation dosed rats.
Conference presentation
Drug Delivery to the Lungs 2016 (Edinburgh, UK)
Characterisation of Interspecies Differences between Human and Rat Airway Macrophage Responses In Vitro.
Association of Inhalation Toxicologists (AIT) annual meeting 2016 (Cambridge, UK)
Development of High Content Analysis Screening Tools to Assess Lung Macrophage Responses In Vitro.
The NC3Rs CRACK IT Challenge: “Inhalation Translation".
APS International PharmSci Conference 2015 (Nottingham, UK)
Adaptation of High Content Assay to Evaluate Macrophage Responses to Inhaled Medicines.
Conference presentation
Drug Delivery to the Lungs 2015 (Edinburgh, UK)
Assessment of Physico-Chemical Properties of Amiodarone Hydrochloride on Alveolar Macrophage Properties In Vitro.
Conference presentation
Association of Inhalation Toxicologists (AIT) 2015 Annual Meeting (Cambridge, UK)
CRACK IT in vitro approaches.
Publication
Hoffman E, Kumar A, Kanabar V, et al. (2015). In vitro Multiparameter assay development strategy toward differentiating macrophage responses to inhaled medicines. Molecular pharmaceutics 12(8): 2675-2687. doi:10.1021/acs.molpharmaceut.5b00048.
Phase 2 awarded
A team led by Dr Ben Forbes, King's College London, has been awarded £1m to deliver the project: Differentiating alveolar macrophage responses to inhaled medicines.
Phase 1 awarded
Four Phase 1 Awards were made to project teams led by:
- Professor Mark Bradley, University of Edinburgh, £98,639.
- Dr Josephine Bunch, National Physical Laboratory, £99,985.
- Dr Ben Forbes, Kings College London, £81,041.
- Dr Victoria Hutter, University of Hertfordshire, £55,050.
Challenge launched
Sponsored by GSK and Envigo, the aim of the Inhalation Translation CRACK IT Challenge is to enable the longitudinal and non-invasive assessment of inflammation and foamy macrophage (FM) toxicity in the same animal through a series of dose-escalation stages. This will require (i) the development of translational tools to assess FM modulation and inflammation in a longitudinal manner in rodent lungs (primarily the rat) and (ii) better insight into FM status and functionality as a response to drug inhalation.
Background
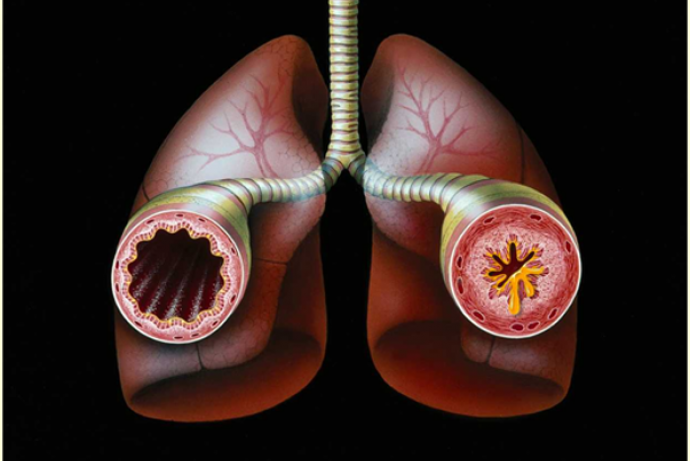
Chronic inflammatory diseases of the airways, such as asthma and chronic obstructive pulmonary disease (COPD), remain areas of considerable unmet medical need. Few new drugs have made it to the clinic during the past 50 years, with many that perform well in preclinical animal studies failing in humans owing to lack of safety and/or efficacy. The failure to translate promising drug candidates from animal studies and other preclinical assays to humans has led to questions about the utility and relevance of current preclinical models and demand for more predictive tools.
Inhaled therapies for asthma were first developed in the 1950s and remain the preferred route of administration for treating the disease because they enable the topical delivery of minute but therapeutically effective doses of drug into the airways eliciting local effects within the lungs. The improved pharmacokinetic profiles and reduced side effects of inhaled therapies also make this a promising route of administration for non-pulmonary indications, e.g. diabetes. Pharmaceutical companies are investing in dry powder delivery devices for inhalation therapies as they offer many advantages over aerosolised solutions. However, preclinical development of inhaled dry powder therapies presents a number of challenges. These can arise through both the poor understanding of the lung response to dry powders and the current inability to effectively monitor efficacy, making dose selection and duration of action assessment particularly challenging.
Animals (mainly rodents) are pre-dosed with candidate drugs and then exposed to a pro-inflammatory challenge (e.g. lipopolysaccharides (LPS)). Lung biopsies or lavage are then examined at defined time points to assess both anti-inflammatory efficacy and toxicity of the compound. This process has a number of limitations and uses a significant number of animals.
One of the difficulties in assessing inhaled drugs in toxicity studies is the alveolar macrophage response and its relevance to safe dosing in the clinic. One characteristic of inhaled dry powder toxicity studies is the appearance of foamy macrophages (FM), but it is unclear if this is due to general particulate overload or a pharmacologically-driven adverse event. This is further complicated when subtle changes in macrophage numbers, appearance and activation are observed, as they may represent an adaptive response to the dosed material, or the initial stages of an adverse health effect. The inability to discriminate between such responses triggers additional in vivo assessments to determine whether there are secondary consequences of FM appearance, such as inflammation, to make go/no-go decisions on candidate drugs. To improve inhaled drug development, a better understanding is required of FM biology, the influence of different macrophage phenotypes on other lung cells and species differences. This knowledge base would reduce costly and repetitive toxicological studies in animals required to optimise safe doses.
3Rs benefits
As an example, a single biology efficacy study using six groups of animals, pre-dosed at a single level over a partial time course requires approximately 60 animals. This might be repeated three times, requiring 180 animals, although the final figure is likely to be many more when full time courses, control groups and multiple studies are taken in to consideration.
Successfully solving this challenge would have the following 3Rs benefits:
- Ability to evaluate toxicity and efficacy longitudinally in the same animal, potentially reducing animal use by up to 90% at certain stages of drug discovery and development.
- More reliable and less variable data resulting in fewer animals being used.
- Earlier go/no-go decisions can be made on drug candidates therefore requiring fewer regulatory toxicity studies in candidates that will fail later in development.
- Potential for similar 3Rs benefits to translate to other therapeutic areas where inhaled therapy could be used (e.g. diabetes, heart failure, oncology).
Phase 1 winners
Project teams led by:
- Professor Mark Bradley, University of Edinburgh, £98,639.
- Dr Josephine Bunch, National Physical Laboratory, £99,985.
- Dr Ben Forbes, Kings College London, £81,041.
- Dr Victoria Hutter, University of Hertfordshire, £55,050.
Phase 2 winner
Project team led by:
- Dr Ben Forbes, Kings College London, £1 million.
Full Challenge information
Assessment information
Through the Inhalation Translation Challenge, the team has developed an in vitro assay and refined in vivo model to reduce the use of animals to identify compounds with the potential to induce inflammation and foamy macrophage toxicity.
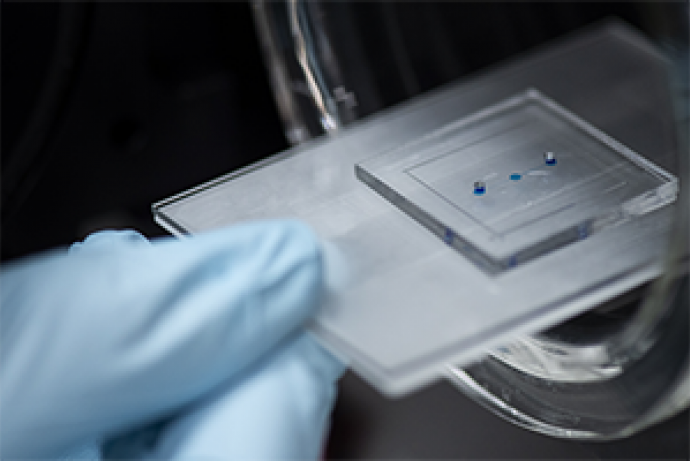
96-well In vitro assay
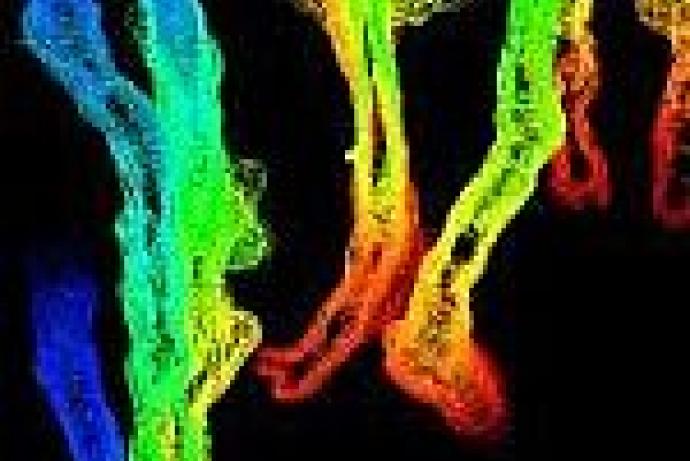
Using a human macrophage cell line (U937) and high content fluorescence imaging analysis, the team has developed a predictive in vitro assay platform which utilises readily available analytical equipment capable of quantifying cell viability, morphometry, and phospholipid and neutral lipid accumulation. The assay methodology has been published and the outcomes have been validated with 20 test compounds of known toxicity potential and 12 compounds provided by the Challenge Sponsors. These data are comparable to data generated in a rat macrophage cell line (NR8383) and primary rat alveolar macrophages obtained by bronchoalveolar lavage. The team has also developed algorithms to predict the likelihood of induced macrophage responses to drug compounds based on molecular properties and the in vitro responses.
A series of complimentary approaches to understand the responses of macrophages include transcriptomic analysis and mass spectrometry imaging to identify drugs, metabolites and lipid changes in lung cells and tissues. These techniques can be used to provide mechanistic insights to underpin empirical observations, provide an opportunity to correlate in vitro and in vivo observations and investigate inter-species differences.
In vivo assay
To monitor responses longitudinally and minimally invasively in preclinical studies, the team has developed a rat exhaled breath analysis approach. Apparatus has been designed to collect samples from animals in standard toxicology studies to provide additional data. Potential biomarkers require validation before this can be offered as a service by study sponsors or service providers.
Morph_ONE
Morph_ONE is a reproducible, mechanistic-driven cell painting assay that can differentiate alveolar macrophage responses in vitro and match them to compounds with varying safety profiles. The data from the assay allows insight into the response of the immune system in the lungs to inhaled chemical products during product development and safety assessment.
Morph_ONE reduces the reliance on classical in vivo inhalation toxicity studies, provides a more detailed understanding of alveolar macrophage responses and data can be compared with a historical in vivo study database to predict product safety.
Using high content image analysis, morph_ONE evaluates the impact of inhaled substances on alveolar macrophages by examining over a dozen morphological features. These features include sphericity, cell and nuclear area, shape analysis and vacuolation profiles, allowing identification of potentially harmful compounds early in the development process.
Features



Access the technology
Find out more about how you could use morph_ONE on the Immuone website or contact the team directly at info@immuone.com.