Transgene Track
The aim of this Challenge was to develop a non-invasive imaging approach to determine the in vivo efficacy and biodistribution of (chimeric antigen receptor) CAR-T cells and adeno-associated viruses (AAVs).
A team led by Professor Wolfgang Weber, Technical University of Munich were awarded funding for this Challenge and developed a platform capable of non-invasive longitudinal monitoring of ATMP-based therapies in vivo, reducing the number of animals required per study. Read more about their work in a 2025 publication: PET-based tracking of CAR T cells and viral gene transfer using a cell surface reporter that binds to lanthanide complexes.
Publication
Morath, V. et al. (2025) 'PET-based tracking of CAR T cells and viral gene transfer using a cell surface reporter that binds to lanthanide complexes', Nat. Biomed. Eng.
Challenge Completed
A team led by Professor Wolfgang Weber, Technical University of Munich have developed a platform capable of non-invasive longitudinal monitoring of ATMP-based therapies in vivo, reducing the number of animals required per study.
Conference presentation
Project developments will be presented at the 16th Annual Meeting of the European Society for Molecular Imaging.
Phase 2 awarded
A team led by Professor Wolfgang Weber, Technical University of Munich, has been awarded £999,999 to deliver Phase 2.
Phase 1 awarded
Project teams led by:
- Dr James Simon, Cenya Imaging BV, The Netherlands, £100,000.
- Professor Wolfgang Weber, Technical University of Munich, Germany, £99,990.
- Dr Tammy Kalber, University College London, £72,183.
Challenge launched
Sponsored by GSK and Novartis, this Challenge aims to develop a non-invasive imaging approach to determine the in vivo efficacy and biodistribution of (chimeric antigen receptor) CAR-T cells and adeno-associated viruses (AAVs).
Background
Cell and gene therapies are emerging treatment modalities that offer new possibilities for the treatment of previously incurable conditions. They can be broadly categorised into two subsets: in vivo gene therapy, which involves the introduction of a therapeutic vector directly into the patient and ex vivo gene therapy, which primarily uses haematopoietic cells to carry the transgenes of interest.
In vivo gene therapy using AAVs
AAV is a common delivery vector for in vivo gene therapy. It has not been associated with disease, is minimally immunogenic, and is able to achieve efficient and long-lived gene transfer, making it an attractive option for gene therapy applications. The number of clinical trials and marketed products based on AAVs is increasing with the percentage clinical trials involving recombinant AAVs rising from 6% to 24% in the last five years 1,2. To date, the FDA have approved two recombinant AAVs (rAAV) for genetic diseases; Luxturna for the treatment of a rare form of inherited retinal disease, and Zolgensma for the treatment of young children with spinal muscular atrophy 3. Currently, more than 230 clinical trials are evaluating the use of rAAV for a variety of conditions, including neurodegenerative diseases, cystic fibrosis, lysosomal storage diseases and blood disorders ((https://clinicaltrials.gov/) and (http://www.abedia.com/wiley/index.html)).
Ex vivo gene therapy using CAR-T cells
Clinical trials for the treatment of cancer have used a number of different ex vivo gene therapy strategies to target the tumour. The modality that has advanced furthest in clinical development is CAR-T cell therapy. Using this approach, patient T cells are genetically engineered to express CARs, which are molecules containing a binding domain specific to the target tumour.
Companies including Novartis and GSK, are evolving new CAR-T therapies targeting different antigens specific for various types of blood cancers and solid tumours. In 2017, the FDA approved the first two CD19 CAR-T cell therapies — Kymriah and YESCARTA.
These landmark approvals have spurred major development in the field, with more than 400 CAR-T cell therapies currently being investigated in Phase I-III clinical trials worldwide (https://clinicaltrials.gov/). The market is anticipated to triple in size, reaching over $8.21 Billion by 2025 4, making it the fastest growing sector in the regenerative medicine industry.
Assessment of safety and disposition
Not all conventional pharmacokinetic parameters (e.g. absorption, distribution, metabolism and excretion) apply to gene therapy. The disposition and persistence of the therapeutic product should be understood prior to first dose in humans as even a single dose of a gene therapy product could persist in the body for a long time (potentially for life). These data may also influence the design of preclinical safety studies (e.g. dose, duration, timepoints etc). In addition, for viral vectors, the possibility of inadvertent germline transmission (vertical transmission) or of shedding (dissemination of the vector into the environment) — with the risk of infection of healthcare professionals or patient’s family (horizontal transmission) — must be addressed. Other potential toxicities can include integration site specific hazards, immuno-toxicity and for CAR-T cells, acute on-target, off-tumour 5, off-target, off-tumour 6,7 and neurological toxicities 8,9,10. The design of the biodistribution studies, as well as the bioanalytical techniques used, will differ based upon the objective of the study.
Immunohistochemical and PCR techniques have been applied to determine the biodistribution, persistence and shedding of gene therapy products into tissues and tumour sites 11,12. However, they require the animals to be euthanised. These analyses also often demonstrate significant heterogeneity and do not provide information on the temporal and spatial localisation of the gene therapy, both within the target tissue and other organs.
Novel approaches that have been developed for biodistribution studies for AAVs include:
- AAV Barcode-Seq — a novel method that allows the collection of high-throughput data on the correlation between AAV capsid sequence and phenotype, with the potential to monitor the biodistribution of several viruses at the same time 13.
- A new AAV vector coding a firefly luciferase and a fluorescent protein in combination with a DNA barcode to optimise data readouts from in vivo studies 14. The presence of the luciferase reporter allows for longitudinal bioluminescent imaging studies, while the use of barcoded capsid variants offers the possibility to track several viruses in the same animal.
- AAV-bcTuD, an AAV expressing barcoded Tough Decoys (bcTuD), which are highly stable RNA transcripts that can be used as readouts for transduction efficiency 15.
A major limitation of these methods is the potential competition among capsid variants for cell receptors that might modify the performance of viruses when used alone. Moreover, the signal from the firefly luciferase used for the in vivo imaging shows low penetration depth and poor quantification capabilities, limiting its use.
Magnetic resonance imaging possesses several advantages that make it suitable for cellular imaging, such as superior soft tissue contrast and high resolution, but so far has only been used for local and not systemic biodistribution of rAAV 16,17.
Approaches that have been developed to track CAR-T cells include:
- High contrast immuno-positron emission tomography (immuno-PET) detecting CD8 protein has previously shown efficacy for tracking the biodistribution of T cells in vivo 18,19. While this approach is useful to detect the total CD8 positive cell population, it does not discriminate between cells that have been transduced by the therapy and those that have not.
- The human sodium iodide symporter (NIS) system for specific high-resolution serial imaging of CAR-T cells, in vivo 20. This technique has potential for translation to the clinic but is restricted because several normal tissues also express the NIS protein.
- Ex vivo labelling of CAR T cells using isotopes (e.g. 89Zr-oxine, In-111 oxine). This also labels the total cellular population and due to isotope half-life, limits the determination of only the initial biodistribution over the first seven days post-dosing 21.
- A recent study used PET tracing to detect prostate-specific membrane antigen (PSMA)-tagged CD19 CAR-T cells in a mouse model of acute lymphoblastic leukemia. Although this approach is a significant step forward in terms of CAR-detection this approach cannot be applied to all cancer models and further work is required to quantify the kinetics of CAR T migration and expansion 22.
The development of a technique to monitor and quantify the kinetics of migration, biodistribution and activity of cell and gene therapy products is critical for both the elucidation of therapeutic efficacy and safety, and to minimise the risk of attrition in clinical trials.
3Rs benefits
The gold standard preclinical in vivo study to assess gene therapy biodistribution, involves necropsy and time-consuming immunohistochemical or molecular analysis of numerous tissue sections or homogenates.
A preclinical viral vector biodistribution study is a core regulatory requirement prior to initiating a clinical trial, and has been recently described in the FDA, EMA and cross-health authority publications 23,24,25. A pilot experiment for the evaluation of one viral vector with three time points and one species would require the use of 15 animals. However, to meet the current regulatory expectations, an average of 40-60 animals are required per study.
At present, there is no regulatory requirement to track the biodistribution of CAR-T cells, but it is desirable to obtain information regarding the effective targeting of the cells to the tumour and the efficacy and persistence of the cells. At the pre-candidate selection stage, GSK runs approximately four studies per year. As an example, in a human tumour xenograft efficacy study in mice, a CAR construct would be evaluated at two different cell doses plus controls, using up to eight animals per group per gender. In order to fully evaluate the dynamics of T cell behaviour, even over a short time period, cohorts of animals would be culled at at least two time points, resulting in 96 animals being used.
A sensitive in vivo imaging technique developed through this Challenge would mean that the same animal could be followed for the whole length of a study, reducing the numbers of animals required by potentially more than 50%. The ability to detect efficacy end points earlier would also reduce study duration, minimising the welfare burden on the animals and deliver cost efficiencies.
In addition, if a reliable method to translate the biodistribution results between species was developed, the requirement to sometimes repeat the same experiments in other species would be removed.
Full Challenge information
Phase 1 winners
Project teams led by:
- Dr James Simon, Cenya Imaging BV, The Netherlands, £100,000.
- Professor Wolfgang Weber, Technical University of Munich, Germany, £99,990.
- Dr Tammy Kalber, University College London, £72,183.
Assessment information
Challenge Panel membership
| Name | Institution |
|---|---|
| Dr Ian Ragan (Chair) | Independent |
| Dr Ashley Hamilton (Sponsor) | GSK |
| Dr Armin Sepp (Sponsor) | GSK |
| Dr Marie Davies (Sponsor) | GSK |
| Dr Silvana Libertini (Sponsor) | Novartis |
| Dr Fraser McBlane (Sponsor) | Novartis |
| Dr Greg Terszowski (Sponsor) | Novartis |
| Dr Uday Phadke | Cartezia |
| Professor Andrew Baker | University of Edinburgh |
| Professor Mimoun Azzouz | University of Sheffield |
| Professor Brian Bigger | University of Manchester |
| Professor Gareth Thomas | University of Southampton |
| Professor Rachel Bearon | University of Liverpool |
| Professor Jurgen Schneider | University of Leeds |
Current methods to study gene therapy biodistribution involve analysing animal tissue at several time points and meeting regulatory expectations for a full preclinical biodistribution study can require 40 to 60 mice. For CAR-T cell studies, evaluating the dynamics of T-cell behaviour even over a short period can involve using large cohorts of animals at multiple time points. These analyses also often demonstrate significant heterogeneity and do not provide information on the temporal and spatial localisation of the gene therapy, either within the target tissue or other organs.
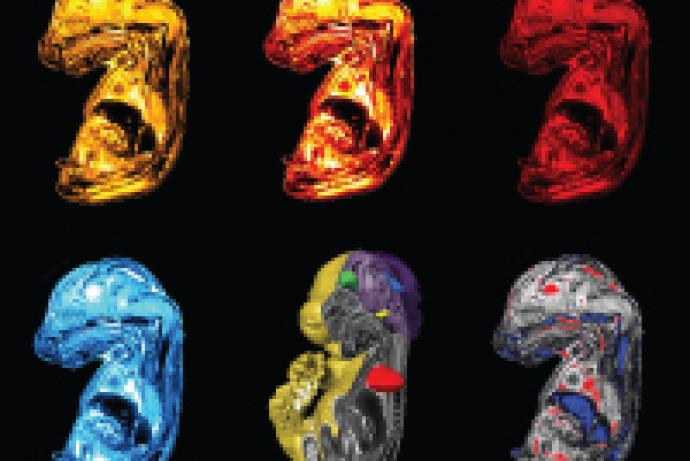
The team at Technical University of Munich, with support from the Challenge Sponsors GSK and Novartis, developed a novel reporter gene system called DTPA-R. The reporter gene is expressed on the surface of modified cells and can be detected in vivo using non-invasive Positron Emission Tomography (PET).
This system allows researchers to track cell and gene therapies in the same mouse throughout a study, reducing the number of animals required. Additionally, the ability to monitor biodistribution in real time allows earlier identification of efficacy endpoints, leading to shorter study durations and minimising the suffering that animals experience. Having a reliable method that supports comparison of biodistribution data across species could eliminate the need to repeat experiments in multiple species, further reducing animal use.
For more information please contact Volker Morath at the Technical University of Munich.
A team led by Professor Wolfgang A. Weber at the Technical University of Munich (TUM) developed a non-invasive PET reporter gene technology (DTPA-R) that enables sensitive and specific in vivo imaging of transgene expression.
The system consists of a reporter gene expressed on the cell surface and a corresponding radioligand ([18F]F-DTPA). The radioligand is injected intravenously and accumulates only in tissues where the reporter gene is produced by cells of the host or the cell therapy product. The accumulation of the radioligand leads to increased radioactivity in this region, which can be detected by PET allowing, for example, the quantification of adeno-associated viral (AAV) gene transfer or chimeric antigen receptor (CAR-)T cells in rodents.
The system enables longitudinal data collection, providing earlier identification of efficacy endpoints that can shorten study durations. Beyond preclinical applications, the technology could be adapted for clinical translation, making it possible to track advanced therapy medicinal products for safety monitoring in humans.
Read the paper, published in Nature Biomedical Engineering, to find out more: Membrane-anchored anticalin enables PET imaging of transgene expression in vivo.
TUM is offering the system to interested academic and industry institutions to help answer important questions in basic research and biopharmaceutical development. For inquiries about the PET reporter, please contact Volker Morath.