Strategic grant
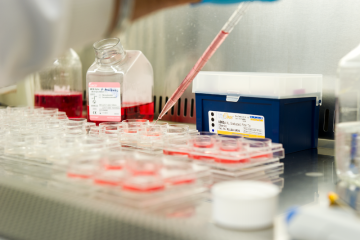
Bioreactor infrastructure for organoid culture in human models of reproductive diseases
At a glance
Completed
Award date
October 2024 - March 2025
Grant amount
£40,772
Principal investigator
Professor Andrew Blanks
Co-investigator(s)
Institute
University of Warwick
R
- Replacement
