PhD Studentship
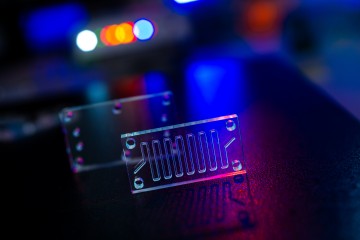
Organ-on-a-chip modelling of respiratory-vascular cell-cell communication in Chronic Obstructive Pulmonary Disease (COPD)
At a glance
In progress
Award date
March 2025 - February 2028
Grant amount
£100,000
Principal investigator
Professor Beata Wojciak-Stothard
Co-investigator(s)
Institute
Imperial College London
R
- Replacement
