Developing liver organoids – from stem cells to tumours
Over the last fourteen years, Dr Meri Huch has built a career developing organoids to study human organs in health and disease. This includes developing the first human liver organoids for preclinical research, most notably enabling liver cancer to be studied in vitro. Meri’s research has been recognised for its contribution to studying the liver by a number of organisations including the British Society for Cellular Biology, the European Molecular Biology Organisation and the International 3Rs Prize. During her three-year NC3Rs Project grant she was invited as keynote speaker at over 20 different workshops, seminars and conferences and the publication detailing the development of liver cancer organoids has been cited over 1,000 times to date.
From mouse to human in vitro liver
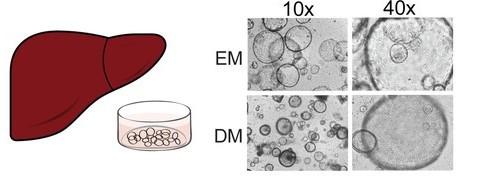
Culturing liver in vitro is challenging as isolated cells undergo de-differentiation in 2D culture, losing performance such as metabolic function over time. Meri was awarded the International 3Rs Prize in 2013 for a publication detailing a novel liver organoid system where cells could be expanded in culture, without de-differentiation, for over a year. This model was significant for numerous biomedical applications, including liver inflammation research, drug metabolism and toxicity studies, as well as transplantation for liver damage and other chronic or inherited liver conditions.
With support from the grant provided with the International 3Rs prize, along with further funding from Wellcome and Cancer Research UK Cambridge Centre, Meri’s team completed the work she initiated as a postdoctoral researcher, and further developed their technology to create human liver organoids1. This development reduced the heavy reliance on in vivo studies for genetic human liver disease research, where a typical study to investigate one drug compound to treat one form of liver disease could require up to 50 animals per experiment.
Creating tumour organoids: Tumoroids
Meri subsequently looked to adapt her human organoid method to model liver cancer. Liver cancer has a poor prognosis, limited treatment options and a heavy reliance on in vivo studies. Cells can be isolated from patient tumour tissue and implanted into immunocompromised mice to form a patient-derived xenograft (PDX) model. These models have successfully been used as a test for therapeutics but are not possible for many patients as the success rate for implantation is low. Additionally, the tumours are formed from multiple cell types with various mutations, which complicates treatment as a single drug may impact different tumours, or parts of the same tumour, differently.t
Using her NC3Rs Project grant, Meri and her team developed a method able to grow tumoroids (mini-tumours) from patients’ own tumour cells. These mirrored the tissue structure and gene expression patterns of the original tumours2. To build confidence in the mini-tumours and demonstrate utility as a drug screening tool, the team tested 29 drugs, already used in the clinic or in development, for their efficacy in treating liver cancer. From this screen, one promising drug was tested in vivo, by transplanting tumoroids into mice to make sure the stromal components were present. The study showed a marked reduction in tumour growth. Overall, the pre-screening allowed Meri and her team to replace the use of almost 300 mice.
During her NC3Rs Project grant, Meri was awarded the BINDER Innovation prize for outstanding cell biological research and a British Society for Cellular Biology Women in Cell Biology Early Career Award Medal. She was also awarded a European Molecular Biology Organisation Young Investigator Programme Award to support her in establishing her own research group. Meri was invited as keynote speaker to over 20 workshops, seminars and conferences across 11 countries during the lifetime of her NC3Rs funding.
Liver dysregulation in disease – infection and cancer
Since her award, Meri received the first Lise Meitner Excellence Program Award from the Max Planck Society to move her research group to the Max Planck Institute of Molecular Cell Biology and Genetics in Germany where she is now a scientific director. Her group focuses on tissue regeneration and its dysregulation in disease predominantly focusing on the liver. Meri’s contributions to organoid research have continued to be recognised, she was awarded the German Stem Cell Network Hilde Mangold Award for outstanding female stem cell researchers and the Allen Distinguished Investigator award to study the turnover and transport of lipids in the liver.
Through developing the liver tumoroids, Meri has become a part of a network of researchers across Germany working on the early detection and prevention of liver cancer. This network was funded by the Federal Ministry of Education and Research, with three projects aiming to identify relevant biomarkers to diagnose and prevent liver cancer at early stages. Meri has continued to apply the human liver organoid and tumoroid methods with collaborators furthering the 3Rs impacts of the model to new areas of liver research. These include hepatitis B infections, co-culture of portal vein and ductal cells, and analysing the impact of impaired bile flow on liver cells.
References
- Huch M et al. (2015). Long-term culture of genome-stable bipotent stem cells from adult human liver. Cell 160(1-2):299-312. doi: 10.1016/j.cell.2014.11.050
- Broutier L et al. (2017). Human primary liver cancer–derived organoid cultures for disease modeling and drug screening. Nat Med 23:1424–1435. doi: 10.1038/nm.4438